

SARS-CoV-2, the virus
The ability to follow and monitor the evolution of the virus, in real time, was one of the greatest competitive advantages to find a way to stop the pandemic and the disease.
Science produced knowledge at an incredible speed, bringing together technology and expertise worldwide. At first we knew little, today much is known about the virus and the disease it causes.
We know that the virus mutates as it reproduces inside the cells of the infected person. This means that the virus is constantly playing a poker game with the person it infects!
There are two important questions in the poker game of the virus evolution:
- What is a good move for a mutant virus to beat another virus?
- What is a good move for a virus to beat the immunological surveillance of the host that it infects?
By learning the rules of the SARS-CoV-2 poker, we have an extraordinary power to end this game.
Monitoring
To watch how the virus changes over time. This can give us basic information: how quickly the virus mutates and what kind of changes are taking place in its genome. This information is critical for previewing its moves.
Evolution
Monitor to break the poker game of the virus and follow its gene. If the virus draws a card that does not change the spike, there is no potential problem! But if he draws a card that changes it is a potential good hand for the virus and we need to follow his next move very early.

Infection
The SARS-CoV-2 virus had to acquire the “correct key” to “open the door” that allows it to enter human cells and replicate itself there.
FAQ´s
The virus and the disease
The new coronavirus called SARS-CoV-2, responsible for Covid-19 disease, was first identified in China, in the city of Wuhan, in December 2019. This new agent had never been previously identified in humans, having caused an outbreak in Wuhan city.
The coronavirus family was first known in 1937 and was specifically described as a corona in 1965, when its characteristics were better known. It gained the name of "corona" because, when observed under the microscope, it was verified that it has the form of a crown. There are dozens of coronaviruses, most of which only infect animals. But coronaviruses were the cause of two recent epidemics that caused severe respiratory syndromes in humans: the 2003 Severe Acute Respiratory Syndrome (SARS) and the 2015 Middle East Respiratory Syndrome (Mers).
The current pandemic is caused by a new coronavirus, called Sars-Cov-2, which started to infect humans in the city of Wuhan, China, in December 2019. When it enters our body, the new coronavirus “sticks” to a protein on the surface of our cells, called ECA-2, as a key that enters a lock. This is where the virus can enter and make our cells work for it, replicating its genetic material and infecting our body.
The virus is transmitted in two ways:
1) from person to person, through droplets (saliva, sneeze, cough),
2) through droplet-contaminated surfaces or objects.
The virus can be transmitted when we stay indoors, close to other people, without wearing a mask. Through affections (kisses and hugs) but also in the exchange of personal objects such as kitchen utensils or the cell phone.
The symptoms most reported in confirmed cases are: fever, cough, muscle pain, headache, generalized weakness or breathing difficulties , loss of smell and taste, nausea, intestinal disorder.
Usually in one week.
Fever, oxygen.
Viruses, as any other microbe, evolve by changing their genomes. This happens because when they make copies of their genomes to produce offspring random errors occur. These are called mutations, the errors that always occur because the copying machine is imperfect and is not able to correct all errors. The coronavirus SARS-CoV-2 has a better copying machine than that of the influenza virus, that is why it is said that it mutates less than the flu virus.
Extra: Our cells have a much better copying machinery, so for each letter in our genome a cell makes 1 error in a billion letters every time it divides. For comparison a coronavirus makes 1000 more errors per letter of its genome.
Protection and diagnostic measures
Protective measures do not eliminate the risk of getting the disease, but the more we apply them, the lower the risk:
- Physical distance
- Use of mask
- Respiratory hygiene (do not cough/talk/sneeze in a person's face)
- Wash your hands frequently
- Hygiene of surfaces and objects.
- Do not exchange personal items: telephone, pens, computers, kitchen utensils, etc.
A single measure may not be enough. The more measures we use, more protected we will be.
It's possible. The virus is spread mainly through the air and closed spaces, such as the elevator, are risk locations. You should avoid sharing the elevator with other people and if possible, you should use the stairs. If it is necessary to use the lift, use suitable protective measures, such as wearing a mask and washing your hands after using it.
Although the virus may be detectable for a few days on clothing, it is not clear that this is a way of transmission. The decision to change clothes depends on the risk associated with what was done in wearing the clothes and how comfortable each person feels with different risks. If you've been with someone with COVID-19 you should change your clothes, on the other hand if you've been walking in a garden without interacting with anyone it's probably not necessary.
Under laboratory conditions viruses can remain on surfaces for several days but there is no evidence of this virus being transmitted through food or packaging. You must have the standard hygiene care for food handling. Wash the food, and wash your hands before and after food preparation.
If the person you exchange bills and coins with is infected there can always be a risk that the money is contaminated. Hands should be washed after handling money.
Public transport are relatively closed spaces and are crowded. They are therefore a risk place for infection. Wear a mask on public transport, wash your hands after using it, and follow general preventive measures.
Children can become infected with the virus and transmit it, although they are less likely to get sick. The importance of children in the spread of the disease is less clear and most likely depends on virus variants and school conditions. Usually schools have protocols and procedures to minimize the transmission of the virus.
Teenagers can also transmit the disease and must follow the same hygiene and behavior rules as adults.
First and foremost, one should always wear certified masks, either through valid CE marking or certificates for social masks issued by various entities (CITEVE, ISQ ect). Currently, due to the presence in the population of the British strain of the virus, in the choice of certified masks, priority should be given to level 2 social masks that have a filtration efficiency of at least 90% of the particles, in detriment of level 3 social masks, with only 70% of filtration efficiency. The masks classified as FFP2 or KN95, although having a higher filtration efficiency of at least 95%, are recommended for health professionals or other professionals who have direct contact with the virus that, due to these functions, need the additional protection conferred by these masks
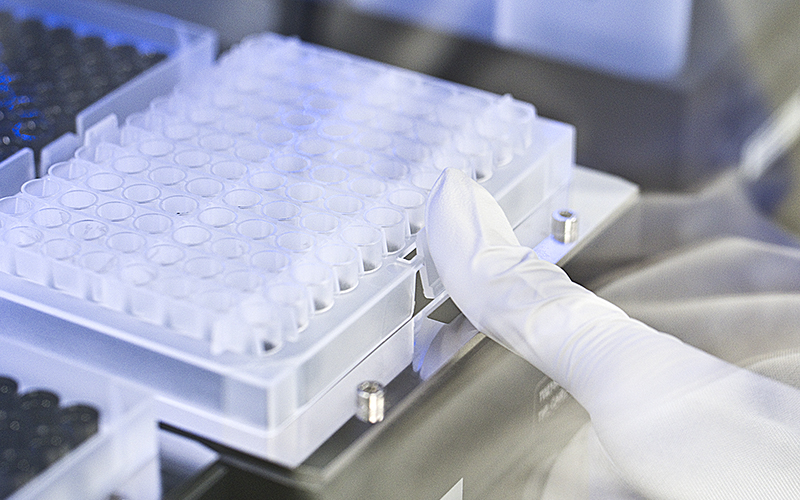
PCR test or antigen test on a swab collection. The same tests on saliva samples are already approved in several countries and used in the context of monitoring.
The virus has an incubation period of about 2-4 days in the host until it can be detected even through the most sensitive tests. Therefore, it means that we can be tested today, with a negative result, and be already incubating the virus. For this reason, it is important to have an isolation period after contacting a positive person. The test answers the question whether we have detectable viruses on the day we were tested. It may happen that hours or a day or two after taking the test we become infected. That's why it's important that we follow hygienic measures to prevent transmission.
This is a complex question because it depends on the level of virus transmission in the community, the type and place of activity of the individual that we are considering, the type of behavior they had, whether they were high or low risk for transmission. Not having risk behaviors, and if the level of virus transmission in the community is low, tests should be carried out when there are associated symptoms or after contacting with a positive case. In case you work in a hospital, in a school, in a factory and the transmission is high, then there is a need to test for symptoms or risk contacts, but it is also advisable to do screening tests once or twice a week according to the established plan.
Testing must be appropriate for the different phases of the pandemic: response (mitigation) and recovery; be integrated into mitigation strategies that are globally defined to reduce the transmission of SARS-CoV-2, be adequate and adapt to the level of transmission in the community. The CDC recommends using two measures to assess community burden and determine the level of transmission risk: total number of new cases per 100,000 people in the past 7 days; and the percentage of nucleic acid amplification test results (NAATs) that are positive during the last 7 days. Both community burden measures should be used to assess the incidence and spread of SARS-CoV-2 in the surrounding community (eg county). The level of transmission to any specific location will change over time and should be re-evaluated weekly for situational awareness and to continually inform planning.
Through serological tests.
6 months.
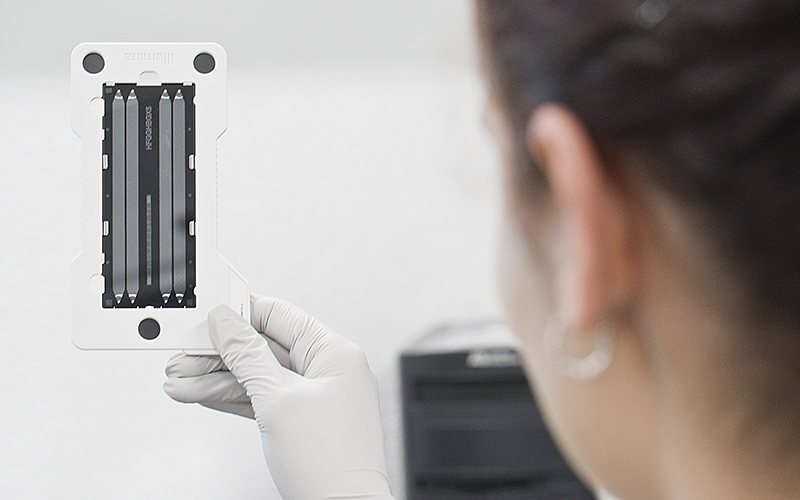
Vaccines
The mRNA vaccine hypothesis was formulated in 1989, when it was shown that mRNA can be delivered to cells when enveloped in a lipid and that it can give rise to a protein. We are hearing about mRNA vaccines now, but that doesn't mean they aren’t the outcome of years of intense scientific work and validation in different areas: cellular biology, immunology, chemistry and pharmaceuticals. It all starts with the discovery of the messenger RNA molecule (mRNA) in 1961. It was necessary to understand how our own mRNA works in our cells, how it could be produced in the laboratory and delivered to the cells of an organism. It was also necessary to understand that our immune system responded to an mRNA administered in this way and to find out how it recognizes and attacks a pathogen in general.
Merix was founded in 1997 as the first company focused on the development of mRNA vaccines, and since then a large number of scientists have studied these vaccines in a range of diseases: viral infections (cytomegalovirus, HIV-1, rabies virus, Zika virus and influenza virus), bacterial infections (Chlamydia, Group A and B Streptococci), parasites (Toxoplasma gondii) and cancer (melanoma and colon carcinoma). In 2012, the first LNP-encapsulated RNA vaccine was described, and several agencies began funding the development of RNA vaccines and therapies. In 2013, for example, the company CureVac in Germany began human trials of a rabies vaccine. The company Moderna, also in 2015, started clinical trials of an RNA-based vaccine for a new strain of avian influenza, which elicited effective immune responses. This same company has started human trials of RNA vaccines for cytomegalovirus (a common cause of birth defects), two mosquito-borne viruses (chikungunya and Zika), and for cancer therapies (solid tumours, lymphoma and melanomas). All studies are in phase 1 or 2, and only the SARS-CoV2 vaccine has been brought to approval. So far, there are more than 20 mRNA-based therapies in clinical trials, in a market whose value has been growing exponentially. The results have pointed to an efficacy and safety of these strategies, although the studies are not yet finished.
The knowledge gathered in several years of studying different coronaviruses has led to a rapid development of a vaccine against SARS-CoV2. The most relevant reasons are:
1) We did not have to discover the structure of the virus or identify which viral protein of SARS-CoV2 allows the virus to enter cells. It was also known that all viruses in this family have on their surface a protein called Spike, which in all cases allows the virus to enter cells.
2) We did not have to identify the human cell receptor that allows SARS-CoV2 to enter cells because the similarity between the SARS-CoV and SARS-CoV2 genomes gave us a candidate that just had to be validated. The Spike protein was found to bind to a protein in our body called ACE2 (Angiotensin-converting enzyme 2) that operates as a receptor for the entry of SARS-CoV, SARS-CoV2 and even NL63-CoV.
3) We didn't have to figure out which viral protein our immune system detects. From years of studying other coronaviruses, we already knew that the Spike protein is the most immunogenic, leading to a potent response triggered by our immune system. Antibodies are part of this response and are proteins that our body produces that recognize the pathogen (or part of it, the antigen). Antibodies allow the virus to enter cells (neutralizing antibodies) or facilitate the action of other components of the immune system. Therefore, it was already known that an effective vaccine would have to give our body directions to produce antibodies against Spike, and that is why almost ALL vaccine strategies against SARS-CoV2 have protein or genetic material in their composition that encodes the Spike protein.
4) There were already many vaccines developed and tested in animals for other coronaviruses. Because of the severity of SARS-CoV and MERS-CoV, many laboratories were already developing therapies, identifying antibodies and testing vaccination strategies against these viruses, to be used if needed.
5) All these studies, which took decades, allowed to reduce the production time of different vaccines against SARS-CoV2. Additionally, during clinical trials there were two critical factors for shortening development time. Phase 1, 2 and 3 clinical trials vary in the number of people to be tested, hundreds, a few thousands and a large number. Usually only the second or third phase is passed, after the first and second, respectively, have been completed and analysed, and after investment by funders. In this case, financing was guaranteed, and so it was possible to test more people at the same time. The other factor is that it takes a long time to test the effectiveness, because it requires the normal course of the infection. Here, as the infection was out of control, it was also quickly possible to determine the effectiveness in protection in a context of natural infection.
6) The platforms for producing vaccines have undergone extraordinary advances (which will be explained below) and different vaccines have been widely tested for other diseases, with robust data on their efficacy and safety.
Vaccines must be produced with the utmost care in order to be effective and safe.
Vaccine manufacturers are able to produce hundreds of millions of doses of flu vaccine each year, and are also able to ramp up production in times of need.
But if 7.8 billion people (the current world population) need a new type of vaccine to protect themselves from SARS-CoV2 and if companies continue to produce the normal amount of vaccines against flu, measles, HPV, rubella and other diseases, there may be a shortage of production. For vaccines that use SARS-CoV2 subunits, and for vaccines that need an adjuvant - molecules added to increase the immune response, there may be a shortage of reagents, such as specific lipids.
Studies indicate that by taking the vaccine you are protected from developing severe disease, they are less clear about protection from infection. We do not know yet for how long the vaccine protects vaccinated people.
The duration of protection for any age group is not yet known because the vaccine hasn’t been administered for very long and there are no data.
Several studies point out that there are some SARS-CoV2 variants for which the vaccine may have less protection, although it is still effective in protecting against severe disease. The case might be that when we are infected by these variants, the vaccine does not protect against infection, but only against the development of severe disease.
News
Partners




